Our Scientific Mission and Vision
Our lab mission is to carry out scientific excellence in microvascular research as a collaborative team.
Our vision is to identify novel signaling mechanisms regulating microvascular endothelial hyperpermeability during sepsis that have potential to be targeted therapeutically for the prevention or treatment of sepsis-induced organ dysfunction. In addition to our research goals, we aim to develop the next generation of biomedical scientists to be creative, innovative, independent, and critical thinkers.
Current Projects
Understanding pathophysiology of sepsis and resulting organ injury
Sepsis is a major clinical problem warranting novel therapeutic approaches. Sepsis is a “life-threatening organ dysfunction caused by a dysregulated host response to infection” with high rates of morbidity and mortality (~30%). Sepsis is characterized by systemic inflammatory response and widespread vascular hyperpermeability leading to edema, organ dysfunction, and death. Other than treating the infection with antimicrobials and attempting to protect organ function and perfusion with fluid, oxygen, and vasopressors, there is no specific strategy to prevent or treat sepsis. Lung injury during sepsis can progress rapidly to acute respiratory distress syndrome (ARDS), a devastating condition of which sepsis is the most common cause, that further increases risk of in-hospital mortality. In addition to lung injury, sepsis often results in multiorgan failure, affecting organs such as the brain, heart, liver, and kidney. A better understanding of molecular mechanisms of sepsis pathophysiology is required to develop targeted therapies for treatment of sepsis-induced organ dysfunction.
Pulmonary microvascular hyperpermeability induced by circulating cell-free hemoglobin or heme
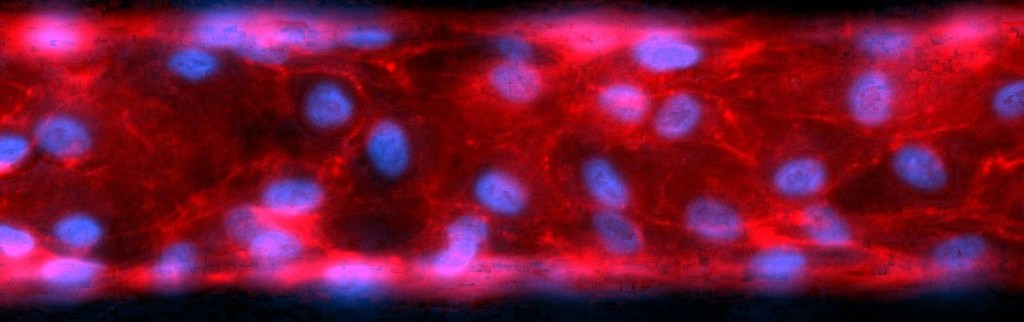
Cell-free hemoglobin (Hb) is a mechanistic driver of microvascular hyperpermeability and lung injury during sepsis. Disruption of the microvascular endothelial cell barrier leading to tissue edema and organ dysfunction is a key pathological mechanism driving sepsis. Several circulating factors during sepsis released from activated immune or damaged cells converge at disruption of the microvascular barrier. Cell-free hemoglobin (Hb) is one such factor, released from damaged red blood cells during sepsis due to their decreased deformability and increased fragility. Though Hb is typically cleared from the circulation by its endogenous scavenger, haptoglobin, stores quickly become depleted in sepsis due to the high levels of Hb released from damaged red blood cells.7 Hb is composed of four globin (two α- and two β-) subunits, each containing a heme group with a central iron atom that can redox cycle from its oxygen-carrying ferrous (Fe2+) form to more reactive oxidized ferric (Fe3+, methemoglobin) and ferryl (Fe4+) forms. Oxidized Hb is susceptible to heme release and is more injurious to cells and tissues than the native form; the oxidative environment produced by activated inflammatory cells during sepsis thus makes circulating Hb and its released heme particularly harmful. Though undetectable in healthy subjects, plasma Hb is elevated in 80% of patients with sepsis and independently associated with mortality and risk of ARDS, making it a feasible target for precision medicine. Selecting patients with elevated levels of Hb or heme for specific targeted therapy holds therapeutic promise for those at risk for sepsis-induced ARDS, but a deeper understanding of downstream mechanisms of heme-mediated lung injury is needed to develop such targeted therapies.
Modulation of microvascular hyperpermeability by scavenger receptors, particularly lectin-like oxidized LDL receptor 1 (LOX-1)
The lectin-like oxidized low-density lipoprotein (LDL) receptor 1 (LOX-1) is a previously unrecognized modulator of pulmonary microvascular endothelial barrier dysfunction. We recently discovered that oxidation of LDL by Hb or heme (heme-oxLDL) exacerbates human pulmonary microvascular endothelial cell (HPMEC) barrier dysfunction through lectin-like oxidized low-density lipoprotein (LDL) receptor 1 (LOX-1). LOX-1 activation signals through several pathways leading to endothelial activation and dysfunction, including increased reactive oxygen species, pro-inflammatory signaling, coagulation pathways, and apoptosis. Moreover, LOX-1 activation promotes self-transcription, perpetuating a positive feedback loop that could enhance endothelial injury. Though LOX-1 is commonly considered the major receptor for oxLDL on endothelium, we have identified that heme itself, as well as several other inflammatory mediators known to be involved in the pathophysiological response to sepsis (advanced glycation end products [AGEs], adenosine triphosphate [ATP], lipopolysaccharide [LPS], palmitic acid [PA], tumor necrosis factor alpha [TNF-α]), upregulate the LOX-1 receptor. This reveals a potentially novel and previously underappreciated paradigm of pulmonary microvascular barrier regulation by LOX-1 that requires further investigation. Additionally, LOX-1 can be cleaved to produce circulating soluble LOX-1 (sLOX-1). Though circulating sLOX-1 has been measured in cardiovascular pathologies, the regulation of LOX-1 ectodomain shedding and its consequences on the lung microvascular endothelium during sepsis are unknown. Moreover, several other scavenger receptors on endothelium may play a role in modulation vascular endothelial injury, including MSR1, COLEC12, SCARB2, and CD36. Our understanding of how these receptors contribute to endothelial barrier dysregulation is just beginning to be explored. Targeting the endothelial LOX-1 receptor and/or other scavenger receptors may represent a new therapeutic avenue for treatment of sepsis-induced ARDS.
Iron dysregulation in pulmonary microvascular hyperpermeability
The implications of intracellular iron dysregulation to pulmonary microvascular hyperpermeability during sepsis are unknown. Pulmonary iron homeostasis is crucial for regulating oxygen transport, cellular respiration and metabolism, oxidant stress, and immune function, and iron imbalances in the lung are associated with respiratory dysfunction. Iron homeostasis in the lung is particularly important due to the lung’s exposure to high levels of oxygen, increasing the risk of injury to lung cells due to iron overload and oxidative stress. Iron overload into the pulmonary endothelium could be especially detrimental in the context of sepsis, as intracellular sequestration of iron is a host defense strategy to limit circulating iron levels available to pathogens (a mechanism primarily studied in macrophages thus far). Without adequate limitation of circulating iron levels, susceptibility of the host to infection increases. In fact, several clinical studies have reported poor prognosis for critically ill patients experiencing iron dysregulation. The role of free iron in heme-related endothelial dysfunction is poorly understood. While several studies point to a critical role for iron in heme-mediated endothelial injury, the data are conflicting. A deeper understanding of the pathophysiological role of iron in mediating pulmonary microvascular hyperpermeability is needed.
Publications
Click Here for Complete Bibliography (Pubmed)
